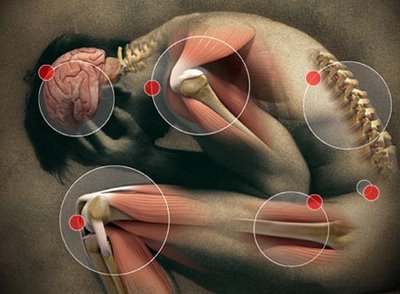
 Fibromyalgia syndrome (FMS or Fibro for short) is a chronic condition, which causes widespread pain and fatigue as well as a variety of other symptoms. The name fibromyalgia comes from “fibro” meaning fibrous tissues (such as tendons and ligaments), “my” meaning muscles, and “algia” meaning pain. The one big problem with this name is that it unfortunately does not really define the whole condition because fibromyalgia is so much more than muscle pain. Fibro is classified as a type of arthritic condition but unlike arthritis, Fibro does not cause joint pain or swelling. The pain from fibromyalgia is produced in the soft tissues of the body, including the muscles and tendons. Because fibromyalgia has few objective signs, and the pain is subjective, it has been called an invisible disability. Certain doctors have even nicknamed it the “irritable everything” syndrome.
Fibromyalgia syndrome (FMS or Fibro for short) is a chronic condition, which causes widespread pain and fatigue as well as a variety of other symptoms. The name fibromyalgia comes from “fibro” meaning fibrous tissues (such as tendons and ligaments), “my” meaning muscles, and “algia” meaning pain. The one big problem with this name is that it unfortunately does not really define the whole condition because fibromyalgia is so much more than muscle pain. Fibro is classified as a type of arthritic condition but unlike arthritis, Fibro does not cause joint pain or swelling. The pain from fibromyalgia is produced in the soft tissues of the body, including the muscles and tendons. Because fibromyalgia has few objective signs, and the pain is subjective, it has been called an invisible disability. Certain doctors have even nicknamed it the “irritable everything” syndrome.
The pain of fibromyalgia is often described as an aching or burning in many areas of the body and is often accompanied by muscle spasms and stiffness. The degree of pain can vary day-to-day and even minute-to-minute, often changing locations and setting up a confusing pattern. In many people with FMS the pain can be so severe that it stops them from performing even simple tasks. This reduction of activity leads to deconditioning and an overall downward spiral of pain and ill health. Many patients with fibromyalgia have to apply for disability because they are unable to work. Others with fibromyalgia are fortunate enough to suffer from only mild discomfort and stiffness. The fatigue that is often associated with FMS is also variable from person to person. Some people with FMS also fit the criteria for Chronic Fatigue Syndrome and often these two syndromes can co exist and are classified together. I have had many patients tell me that the fatigue can become so bad that they feel like they have a continual flu. Thankfully research has shown that Fibro is not usually progressive, not physically crippling, nor does it decrease a person’s expected life span.
 One of the biggest problems and injustices that has occurred for those suffering from fibromyalgia is the fact that for so many years it has been totally undiagnosed or dismissed by many in the medical community. When I first became affected with Fibro back in 1996, there was little information on this condition and although I knew exactly what I had, many looked at my extensive research and passion in a dismissive way. Now that tide has finally turned and we hear fibromyalgia being talked about constantly. We have all seen those commercials for medication for the treatment of fibromyalgia by now and I am happy that at least there is vindication for those who have suffered for so long and felt alone. It is truly amazing when you read the statistics of those affected with this condition that more attention was not given to fibromyalgia sooner. The numbers are staggering and the cost is incredible and the injustices felt by many will be difficult to forget.
One of the biggest problems and injustices that has occurred for those suffering from fibromyalgia is the fact that for so many years it has been totally undiagnosed or dismissed by many in the medical community. When I first became affected with Fibro back in 1996, there was little information on this condition and although I knew exactly what I had, many looked at my extensive research and passion in a dismissive way. Now that tide has finally turned and we hear fibromyalgia being talked about constantly. We have all seen those commercials for medication for the treatment of fibromyalgia by now and I am happy that at least there is vindication for those who have suffered for so long and felt alone. It is truly amazing when you read the statistics of those affected with this condition that more attention was not given to fibromyalgia sooner. The numbers are staggering and the cost is incredible and the injustices felt by many will be difficult to forget.
 Several studies, including resources from The American College of Rheumatology and also the John Hopkins University of Medicine estimate that Fibromyalgia Syndrome affects approximately 3-4% of the population of the USA (10 million – 12 million) or up to 6% of patients seen in doctor’s offices. According to one study done by I. Jon Russell, et al., healthcare costs range from $12 – $14 billion per year for Fibro patients alone and account for a loss of 1% – 2% of the nations productivity. This study also showed that annual costs for fibromyalgia claimants were more than twice as high as those of typical insurance beneficiaries. As you can see this condition imposes not only great pain but also a huge financial burden on the system. Considering the financial condition we face with health care and the crisis we are in, it becomes all the more important for us to properly address this syndrome. Yet this situation has yet to turn around sufficiently because often FMS patients are misdiagnosed or still “dismissed” and go from doctor to doctor seeking help and looking for answers. They become subjected to a barrage of tests that are often unnecessary or repetitious. It is my belief as well as many other experts that the number of fibromyalgia sufferers is actually much greater because many remain still undiagnosed or misdiagnosed and are still searching for answers to their pain. Much of the research shows that approximately 75% – 80% of those diagnosed with fibromyalgia are women. There is now some evidence of a genetic predisposition on the female side of the family.
Several studies, including resources from The American College of Rheumatology and also the John Hopkins University of Medicine estimate that Fibromyalgia Syndrome affects approximately 3-4% of the population of the USA (10 million – 12 million) or up to 6% of patients seen in doctor’s offices. According to one study done by I. Jon Russell, et al., healthcare costs range from $12 – $14 billion per year for Fibro patients alone and account for a loss of 1% – 2% of the nations productivity. This study also showed that annual costs for fibromyalgia claimants were more than twice as high as those of typical insurance beneficiaries. As you can see this condition imposes not only great pain but also a huge financial burden on the system. Considering the financial condition we face with health care and the crisis we are in, it becomes all the more important for us to properly address this syndrome. Yet this situation has yet to turn around sufficiently because often FMS patients are misdiagnosed or still “dismissed” and go from doctor to doctor seeking help and looking for answers. They become subjected to a barrage of tests that are often unnecessary or repetitious. It is my belief as well as many other experts that the number of fibromyalgia sufferers is actually much greater because many remain still undiagnosed or misdiagnosed and are still searching for answers to their pain. Much of the research shows that approximately 75% – 80% of those diagnosed with fibromyalgia are women. There is now some evidence of a genetic predisposition on the female side of the family.
The exact cause of fibromyalgia is unknown, however researches have identified some clues that may explain how certain people develop this syndrome. At times, FMS can develop post traumatically. There are some doctors that believe it originates with some kind of virus that affects the immune system and causes a cascading effect to occur. Other people develop fibromyalgia after sustained stress or long periods of insomnia. There is no truth however that this is a purely emotional or psychological condition. Even if the actual Fibro initially developed because of severe emotional stress, it becomes manifest as a physical condition. I like to explain it to my own patients this way “psychology can often become physiology”. We can also look use this analogy. An acute myocardial infarct (heart attack) can be brought on by severe stress but once the patient has an MI we surely can’t tell them it is “just stress”. More theories on the cause of FMS include a change in several neurochemicals or neurotransmitters. 3 important ones are substance P, nor epinephrine and serotonin. There has actually been some studies that show that substance P, which is located in the spinal fluid and allows us to feel pain, has been several times the normal level in people with Fibro. That is one of the reasons why FMS sufferers feel pain more intense.
Without getting too complex, there are 3 glands within the body that communicate with each other and help the body maintain a normal chemical balance. Those 3 glands are called the HPA axis or the hypothalamus, pituitary and adrenals. For reasons that are not yet well understood this axis becomes disordered and starts a cascading affect. It is therefore widely recognized that people with FMS have neurotransmitter imbalances causing what is known as an upregulation of the autonomic nervous system. Some researchers have called this condition a dysautotomia, which basically means that the autonomic nervous system is out of balance. People with fibromyalgia have muscle spasms and contractions caused by guarding and or splinting from tender points deep within their muscle fibers. These muscular contractions lead to areas of the spine being fixated and subluxated which adds to the problem tremendously. If the muscles in the limbs are splinting a person can have skeletal imbalances in the extremities, which just compounds the problem.
It is important to mention that there is another condition that often co exists with fibromyalgia known as CMP or chronic myofasical pain. This use to be called myofascial pain syndrome but this has recently been changed. To some less familiar with the treatment of these conditions the difference between the two may seem confusing or worse, insignificant. The reason I say that is because there are major differences between FMS and CMP and they should not be treated or managed the same way.
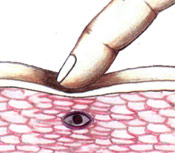 The easiest way for a practitioner to differentially diagnose FMS from CMP is to palpate for sensitive points in the musculature and see if pressing on those points refers pain elsewhere. In fibro, patients have “tender points” that do not refer pain elsewhere. With myofascial pain, a patient will have what are known as “trigger points”, which will refer pain in a specific pattern when pressed. These may seem like subtle differences but often to an experienced practitioner they are quite remarkable. Fibromyalgia sufferers also have a host of other symptoms that go along with their muscle pain. The CMP patients usually have no systemic complaints and often their pain is regional not all over as in fibromyalgia.
The easiest way for a practitioner to differentially diagnose FMS from CMP is to palpate for sensitive points in the musculature and see if pressing on those points refers pain elsewhere. In fibro, patients have “tender points” that do not refer pain elsewhere. With myofascial pain, a patient will have what are known as “trigger points”, which will refer pain in a specific pattern when pressed. These may seem like subtle differences but often to an experienced practitioner they are quite remarkable. Fibromyalgia sufferers also have a host of other symptoms that go along with their muscle pain. The CMP patients usually have no systemic complaints and often their pain is regional not all over as in fibromyalgia.
